"There'll be PhDs written on the psychology and politics of this topic"

A lack of research and old medical dogmas have caused deadly delays in public health bodies accepting that COVID-19 is being transmitted through the air, says aerosols expert Lidia Morawska
10th Nov 2020
Interview by Tom Ireland
Professor Lidia Morawska is the Director of the International Laboratory of Air Quality and Health at Queensland University of Technology in Australia. She has been instrumental in persuading public health organisations that COVID-19 can be transmitted in the air via respiratory particles small enough to float and travel far from their original source – usually droplets of around 5μm (micrometers) and less.
In July Morawska and fellow aerosol scientist Professor Donald Milton published a commentary signed by an international group of 237 other scientists urging public health bodies to acknowledge airborne transmission and take preventive measures to reduce the risk.
After much debate, last week the US Centre for Disease Control updated its guidance to reflect that this transmission route is possible, having briefly published and then retracted similar guidance last month. The World Health Organization (WHO) has agreed that aerosol transmission is possible in some circumstances, but it says there is no new evidence to suggest this is how the virus is spreading.
Morawska says that airborne transmission appears to be the only plausible explanation for several superspreading events where precautions to prevent large droplet or fomite [surface] transmissions had been followed.
She argues that small steps to improve ventilation and air flow in indoor spaces could help reduce the risk in countless buildings across the world.
“While the evidence is still incomplete, under the precautionary principle, we must address every potentially important pathway to slow the spread of COVID-19,” she and her co-authors wrote. “The measures that we propose offer more benefits than potential downsides, even if they can only be partially implemented.”
Hi Lidia. We are almost eight months into this pandemic, and public health organisations have only just started to acknowledge that COVID-19 can be transmitted through the air via aerosol particles. There has been remarkable progress in understanding other aspects of SARS-CoV-2 and COVID-19 – why is it taking so long to reach a consensus on this issue?
I suspect there will be several PhDs written on this particular topic to answer this question and the psychology and politics around it. It's an issue that has been going on for a long time.
During the SARS epidemic in 2003, I was invited by the World Health Organisation to join a team in Hong Kong to explore what happened in Amoy Gardens [where SARS infections spread throughout an estate of high-rise residential towers]. That expedition didn't take place in the end because by then, the epidemic was over. But I started looking into the topic of airborne transmission and I realised to my absolute amazement that there was barely any science at all.
There were hardly any studies done on aerosol particles – or however we term very small droplets from human expiration – and the content of pathogen found in them. Even if we're talking about flu and the common cold, there was hardly any research into how those actually spread through the air.
We wanted to continue fundamental studies on the size and distribution of particles from human respiratory activities, to understand the dynamics of these in the air and how to minimise what there is in the air. But by that stage SARS-1 was a distant memory and absolutely no one was interested in funding this area of research. What's more, when we applied for grants comments from the assessors were of the nature that airborne transmission was not possible – and if airborne transmission is not possible, why research it?
So, we started this pandemic with very little research on the transmission of viruses by aerosol, and a suspicion that it was not really possible.
Yes. Now, the question is why was this? The lack of understanding appears to go back to an old medical dogma, which was based on some studies from the 1930s and 1940s which concluded that if you were at arm's length from an infected person you were safe. But these studies investigated large droplets which fall by gravity very soon after they expired. The researchers even mentioned that the methods available only allowed them to study larger droplets. They didn't say that airborne transmission of anything smaller is not possible – they simply didn't have means to study it.
But this was how that medical dogma was born, that beyond an arm’s length it was safe because the droplets all to the floor. This continues. At the beginning of the pandemic the WHO Director General tweeted that ‘the virus is not airborne’ – it was just as blunt as that.
 The ubiquitous 'Two Metre-Rule' is based on the assumption that COVID-19 is mostly transmitted via larger respiratory droplets which quickly fall to the floor after being exhaled. Smaller respiratory particles can linger in the air and travel much further.
The ubiquitous 'Two Metre-Rule' is based on the assumption that COVID-19 is mostly transmitted via larger respiratory droplets which quickly fall to the floor after being exhaled. Smaller respiratory particles can linger in the air and travel much further. So can you tell me a little bit about some of the studies that have been done since that suggest otherwise?
Well, it's not a huge body of studies. During a pandemic, preparing and starting studies like this is not something you can do easily. You have to have a reasonably sophisticated system, you have to have volunteers with COVID and ethical clearance. When you are in lockdown, that's basically not possible.
There have been a number of studies investigating the presence of aerosols in hospital or healthcare settings, where you have a source of infected people. There was a study done in Florida where they measured concentration and size distribution of particles in the air of a hospital, analysed the viral load in three different size ranges. They showed the highest viral load, or concentration of the virus, was actually in the smallest particle, in the size range below one micrometre (1μm). I was also part of a study conducted in Beijing and in Wuhan where we showed that the virus is present in the air and in exhaled breath.
However, in many medical facilities, while you find some virus in the air you may not find a lot, or it is undetectable. But that could be because usually medical facilities in developed countries have good ventilation. So if you don't detect the virus in the air in hospitals, it doesn't mean that the transmission doesn't exist – it’s that they have exactly the ventilation in place that we are calling for.
Studies of outbreaks also suffer from the limitations of being retrospective studies – you cannot study an outbreak as it starts. Researchers can’t rigorously assess all the parameters about where people were and what the ventilation was like.
However, a body of studies is growing that basically point to airborne transmission as the main mode of transmission now, particularly where people are obeying the recommendations such as social distancing and hand washing. If these measures are in place, how does the virus spread other than airborne transmission? Alongside two groups of colleagues we studied the choir practice event in Washington State where about 45 people were infected from around 60 participants. Using two different modelling methods both of these simulations showed that this could only really be explained by aerosol transmission.
How well do cloth masks help prevent someone dispersing aerosol particles into the air?
Anything you put in front of your mouth helps. We conducted a study several years ago that was on the emissions of people with cystic fibrosis, who are often infected with Pseudomonas. We used the setup which we used for our earlier studies on this and surgical masks, N95 masks and even what we call called etiquette, or coughing into your elbow, showed some benefit.
The question of how much helps? It depends on the quality of the material. It's got to be more than one layer, but also very importantly, the looser the fit or the worse the fit, of course the worse the performance. But still, it can reduce the emission of aerosols and reduce the inhalation.
Is there any evidence to suggest there is a link between aerosol transmission and the severity of the illness?
If you are in proximity to somebody and inhaling emissions containing both small and large droplets you can’t distinguish which is which. But the small droplets can go very deeply into the respiratory tract. Now I'm moving outside my area of expertise – I’m not a virologist – but what I understand is that when they get deeper, then the infection can be more severe.
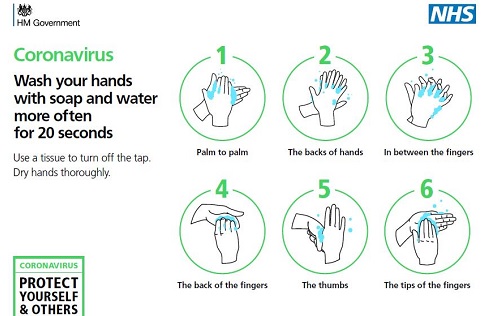 Public health messaging in the early stages of the pandemic focused on hand washing to preventing transmission from surfaces and objects.
Public health messaging in the early stages of the pandemic focused on hand washing to preventing transmission from surfaces and objects. Going back to what we were talking about originally – the psychology and politics involved in taking airborne transmission seriously. Do you think that the many public health organisations and Governments were reluctant to take airborne transmission seriously because it is so much more worrying and difficult to control?
There were medical doctors who were advising the WHO that it is not a significant mode of transmission. So, that was one element. Another element of this was about resources, or rather a lack of resources. In the earlier stages of the pandemic the WHO advised that the general public did not need to wear a mask. Apparently, this was related to the fact that masks were not available. I think that was the wrong approach, because if you say that masks are not needed, then the market doesn't follow and masks still won't be available. And it was hiding the truth, of course.
Masks are one element of this and are the responsibility of individuals. However, when we are talking about building engineering measures – ventilation, flow direction, building design – this is not the responsibility of the individual. This is something which the appropriate government bodies have to recommend or mandate. And so this is something which many governments don’t want to hear about.
 The UK's public health messaging remains focused on preventing surface transmission and transmission by larger droplets.
The UK's public health messaging remains focused on preventing surface transmission and transmission by larger droplets. You are an aerosols expert. When you walk into an environment what are you looking at in terms of things that are going to help lessen your risk of contracting COVID-19?
It is about making sure that there's delivery of fresh air, which means dilution of the virus or any pathogen from the air. The air flow direction is also important; for example, there have been outbreaks on aeroplanes and on buses – even though the ventilation rate is very high, or the air is filtered and recirculated, if it also flows from one person to another, and if that happens for prolonged periods of time, like during long flights, then infection is likely.
This is something I've been doing well before COVID-19. I wore masks in family situations when I had a cold, or when I noticed that one of the family members was sick. It wasn’t socially acceptable to make my PhD students go home when they had a cold, but I would think about how to locate them so the air flow wasn’t going from them towards everyone else.
Now, I look at restaurants, public places, and think ‘is this place ventilated?’ Many restaurants don't seem to have any ventilation, apart from an air conditioner, which doesn't necessarily ventilate but just recirculates the air. So, yes, I'm looking at such equations when I enter a place to determine whether the situation is safe.
Professor Lidia Morawska is the Director of the International Laboratory of Air Quality and Health at Queensland University of Technology in Australia. She is a Professor in the School of Earth and Atmospheric Sciences, Faculty of Science & Engineering, Queensland University of Technology.